

If you have high blood pressure that is not responding to standard medications your doctors may suggest tests for aldosterone and renin.
Up to 20 percent of people with resistant high blood pressure have a condition known as primary aldosteronism in which they have high levels of aldosterone in their blood due to problems with their adrenal glands.
In another condition, called secondary aldosteronism, high aldosterone levels are caused by a range of different health disorders. It is very common in congestive heart failure and almost all cases of cirrhosis of the liver with ascites cause high renin levels, which increases production of aldosterone. It is also common in chronic kidney disease, renal artery stenosis (narrowing of one or both arteries that carry blood to the kidneys) and pre-eclampsia in pregnancy.
Diagnosing aldosteronism is important because it represents one of the few causes of high blood pressure that is potentially curable. It can sometimes be difficult to diagnose because many people only have vague symptoms or no symptoms at all. This means the condition can go unnoticed unless specific testing is done.
A quick look at blood pressure
Blood takes oxygen and nutrients to all parts of your body. Your beating heart helps to push blood through a network of blood vessels – arteries and veins. Your blood vessels are constantly adjusting, contracting or relaxing, becoming narrower or wider to keep your blood pressure stable and blood flowing.
Your blood pressure goes up and down in response to things like exercise, eating, stress, medications and underlying health conditions. Problems arise if your blood pressure stays too high for too long.
High blood pressure, called hypertension, makes your heart work harder than normal and over time this weakens the heart muscle. The increased pressure of blood flow can damage your blood vessels, making them stiff or narrower and this increases the risk of blood clots.
Blood pressure is the measure of the force of your blood as it pushes against the walls of your arteries.
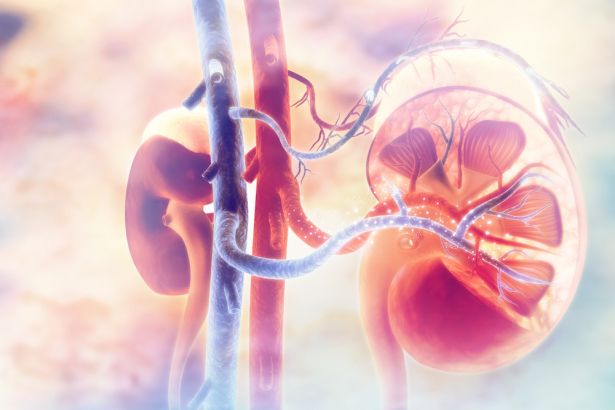
How your kidneys help control blood pressure
Your kidneys are located just at the bottom of your ribcage on either side of your spine. Inside each kidney are about a million tiny blood filtering units. These filter your blood and remove wastes and excess water from your body. Water is sent to your bladder to be removed as urine.
When your kidneys filter out water from your blood, the amount of water that is kept in your bloodstream and the amount that is passed into your urine to be removed can be adjusted.
Sodium
Your kidneys use sodium as a way of controlling how much water stays in your blood and therefore, how much blood volume and blood pressure you have.
The kidneys’ tiny filters pull sodium out of the urine and into the bloodstream. Water naturally moves towards areas where there is sodium in a process called osmosis. When sodium moves back into the blood, water follows. This extra water increases blood volume and raises blood pressure. For more see Sodium.
Potassium
The electrolyte potassium works in the opposite way to sodium, and it helps the kidneys get rid of excess sodium from your bloodstream through your urine. Potassium also directly affects your blood vessels. It causes them to relax and widen making it easier for blood to flow lowering blood pressure. For more see Potassium.
Aldosterone
Aldosterone is a hormone that helps the body to maintain normal blood pressure. It does this by enabling the kidneys to hold on to salt (sodium) while getting rid of potassium which is passed into the urine.
Aldosterone is made by the adrenal glands which sit on top of the kidneys, and the amount that is produced is controlled by renin, an enzyme made by the kidneys.
Primary aldosteronism occurs when one or both adrenal glands make too much aldosterone which leads to too much salt and water being retained in the body, causing high blood pressure. In some people this can also lead to low blood potassium levels.
How aldosterone and renin help control blood pressure
The renin-angiotensin-aldosterone system (RAAS) is a complex feedback system of hormones, enzymes and proteins that helps control your blood pressure.
Primary aldosteronism
About 30 – 40 percent of primary aldosteronism cases are caused by benign (non-cancerous) adrenal tumours. This is known as Conn’s syndrome. About 60 – 70 percent are due to both adrenal glands being overactive in a condition called bilateral adrenal hyperplasia. There are other less common causes and rarely, it is caused by cancer of the adrenal gland. There are hereditary types of primary aldosteronism, but these are also rare and most often seen in people younger than 20 years with a family history of stroke and hypertension.
Secondary aldosteronism
Unlike primary aldosteronism, this is caused by problems outside the adrenal glands.
Too much aldosterone can be the result of anything that increases renin levels, such as congestive heart failure, cirrhosis of the liver with ascites, chronic kidney disease, renal artery stenosis (narrowing of one or both arteries that carry blood to the kidneys) and pre-eclampsia in pregnancy.
Secondary aldosteronism is more common than primary aldosteronism and it is important to know which you have as your treatment will be different.
Hypoaldosteronism
A lack of aldosterone, called hypoaldosteronism, usually occurs as part of adrenal insufficiency (Addison's disease). It causes dehydration, low blood pressure, hyperkalaemia (high potassium), hyponatraemia (low sodium) and skin pigmentation.
Blood tests for both aldosterone and renin are usually ordered together when you have high blood pressure, especially if test results show you also have a low potassium level.
Even if potassium is normal, testing may be done if typical medications are not controlling your high blood pressure or if you have had high blood pressure from an early age. Sometimes aldosterone and renin testing is used to clarify the best treatment for high blood pressure.
Aldosterone testing, along with other tests, is also requested if your doctor suspects that someone has a condition called adrenal insufficiency, known as Addison’s disease. This is when the adrenal glands do not make enough hormones, particularly cortisol, and sometimes aldosterone as well.
Sample
Blood
Any preparation?
Collecting a blood sample for aldosterone testing requires careful preparation because aldosterone levels are very sensitive to posture, salt intake, time of day and medications.
Both aldosterone and renin are highest in the morning and vary throughout the day.
Blood is collected in the morning, at least two hours after getting out of bed.
You may be asked to arrive well before your testing time so you can remain in a lying or upright position while the blood sample is being collected.
The amount of salt in the diet and medications, such as non-steroid pain relievers like Ibuprofen, diuretics (water pills), beta blockers, steroids, blood pressure medications and oral contraceptives can affect the test results. Stress and strenuous exercise may also alter the results.
Your doctor will tell you if you should change the amount of salt in your diet, your use of medications or your exercise routine before aldosterone testing.
Aldosterone levels fall to very low levels in severe illness, so testing should not be done when a person is very ill.
Liquorice may mimic aldosterone's properties and should be avoided for at least two weeks before the test. This refers only to products made from the extract of the liquorice root. Most liquorice sold in Australia is flavoured confectionary and does not contain liquorice, but some products do. Check the package label if you are not certain or bring a package with you to ask your doctor.
Reading your test report
Your results will be presented along with those of your other tests on the same form. You will see separate columns or lines for each of these tests.
| Renin and aldosterone (and often cortisol) are measured in order to get a complete picture of what is happening. | |||
| Condition | Aldosterone | Renin | Cortisol |
| Primary hyperaldosteronism (Conn’s syndrome) | High | Low | Normal |
Secondary hyperaldosteronism (Causes of high aldosterone other than the adrenal glands) | High | High | Normal |
| Cushing’s syndrome | Low-normal | Low | High |
| Adrenal insufficiency (Addison's disease) | Low | High | Low |
Reference intervals - comparing your results to the healthy population
Your results will be compared to reference intervals (sometimes called a normal range).
If your results are flagged as high or low this does not necessarily mean that anything is wrong. It depends on your personal situation.
Reference intervals for aldosterone and renin vary between laboratories so you will need to go through your results with your doctor, who will interpret the results based on the reference intervals provided by the laboratory.
Further testing
If your results show primary hyperaldosteronism, you may need more tests to confirm the diagnosis.
Aldosterone Suppression Test
A saline infusion test can be used to see if the aldosterone levels fall when your body levels of salt are high.
CT scan
This will look at the size and shape of your adrenal glands to help identify the cause of your high aldosterone levels.
Adrenal venous sampling
Looking for cell changes and thickening of the adrenal glands (hyperplasia) can be tricky because the size of normal adrenal glands can vary significantly from one person to another. If adrenal hyperplasia is suspected, you may be asked to have adrenal venous sampling. Adrenal venous sampling is done to determine which adrenal gland is making too much aldosterone.
In this test, a radiologist inserts a thin catheter (tube) through a vein in your groin or neck and guides it under X-ray to the veins draining each adrenal gland.
Blood samples are collected from:
The samples are tested for aldosterone. Sometimes cortisol is also measured, and an aldosterone / cortisol ratio calculated. The results from the two adrenal glands are compared. If they are significantly different, then it is likely the problem is in the gland with the highest aldosterone concentration causing primary aldosteronism.
The choice of tests your doctor makes will be based on your medical history and symptoms. It is important that you tell them everything you think may help.
You play a central role in making sure your test results are accurate. Do everything you can to make sure the information you provide is correct and follow instructions closely.
Talk to your doctor about any medications you are taking. Find out if you need to fast or stop any particular foods or supplements. These may affect your results. Ask:
Pathology and diagnostic imaging reports can be added to your My Health Record. You and your healthcare provider can now access your results whenever and wherever needed.
Get further trustworthy health information and advice from healthdirect.